Updated: May 1st, 2023
Published: March 17th, 2023
Updated: May 1st, 2023
Published: March 17th, 2023
Regulations Your Ambulatory Surgery Center (ASC) Needs to Know About
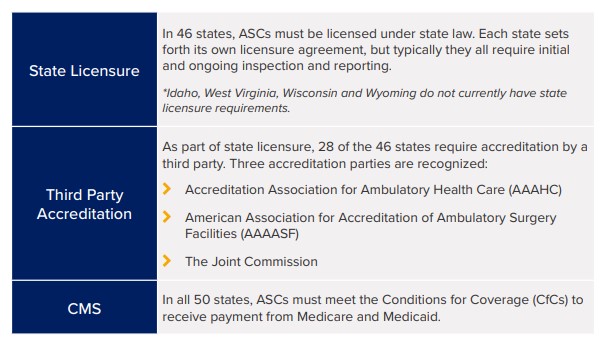
There are just under 10,000 ASCs in the U.S. Each one is required to have some type of credentialing and privileging process in place. Some states are governed by state licensure, others require third party accreditation, and some must comply with both. In all 50 states, ASCs must meet the Centers for Medicare and Medicaid Services’ (CMS) Conditions for Coverage (CfCs) to receive payment.
Current Stats:
- Only 60% of ASCs have met CMS’ CfCs
- 930 ASCs are accredited by The Joint Commission
- 835 ASCs are accredited by the AAAHC
- 168 are accredited by the AAAASF
*Note: All accrediting organizations align their requirements with CMS’ CfC which allows ASCs to receive “deemed status” with Medicare and Medicaid once they are accredited. This means that if you are accredited, for example, by The Joint Commission, you’re also deemed to be in compliance with CMS’ CfC.
All Accrediting Organizations Have Requirements in Place Around Credentialing and Privileging
Credentialing is an umbrella term used by many organizations to summarize the process of obtaining, verifying, and assessing the qualifications of a practitioner to provide care or services in or for a health care organization. Privileging is a subset of the credentialing process whereby a healthcare practitioner is authorized to provide a specific scope of patient care services based on an evaluation of the individual’s credentials and performance. A privilege is defined as an advantage, right, or benefit that is not available to everyone, enjoyed by a relatively small group of people, usually as a result of education and experience.
Credentialing and Privileging is a Top Challenge for Today’s ASC
Credentialing and privileging are a heavy lift. If you’re struggling with these processes, you’re not alone. A recent article published in Becker’s ASC REVIEW notes that The Joint Commission identified the following as the top three challenges facing today’s ASCs:
- Infection prevention and control
- Medical equipment disinfection
- Physician credentialing
Making sure that there is someone within your ASC who’s maintaining your credentialing and privileging, reviewing records, securing evidence of current licensures, etc. and having a consistent process to do so are key to establishing and maintaining compliance.
The Journey Towards Clinical Competency
If you have any doubt at all about your ASC’s ability to perform proper credentialing and privileging, your alarm bells should be ringing. In addition to being required by all accrediting organizations, credentialing and privileging is also vital to patient safety and risk management. Your journey towards clinical competency begins with gaining an understanding of the requirements in place and implementing a process to enable you to deliver against those requirements.
When it comes to Privileging, all accrediting organizations require the following:
- Each ASC must have a governing body in place that is responsible for all privileging decisions. In some cases, this might be just one person, such as the owner of the ASC, but this individual must make all privileging decisions.
- All ASCs must have clearly defined credentialing and privileging policies and procedures that identify:
- The scope of the care your organization is providing
- Who is required to be credentialed and/or privileged to deliver those services
- The qualifications that a provider must possess to be privileged to practice those services in your facility, such as education, training, experience, board certification, etc.
- A process for verifying the qualifications required
- A process for making privileging decisions (Credentials Committee or other authorization pathway)
It’s important to note that providers must be credentialed and privileged upon hire and every two years after that (except in Illinois, where it is required every three years). Reappointment requires data to demonstrate performance within your ASC, which will be used to support current competency.
The Role of a Credentials Verification Organization
There is a reason many hospitals have entire departments dedicated to credentialing – it’s a time-consuming process. In some cases, outsourcing the process may be your best option. ASCs can contract with a credentials verification organization–commonly called a CVO–to obtain primary source verification. A CVO is defined as any organization that provides information on an individual’s professional credentials. If your ASC bases a decision in part on information obtained from a CVO, it’s important that you have a high level of confidence in the completeness, accuracy, and timeliness of the information provided. ASCs are not permitted to grant privileges based on the fact that a provider might have privileges somewhere else. All ASCs must make their own decisions and these decisions need to be based upon data that they have either collected themselves or have received from a CVO.
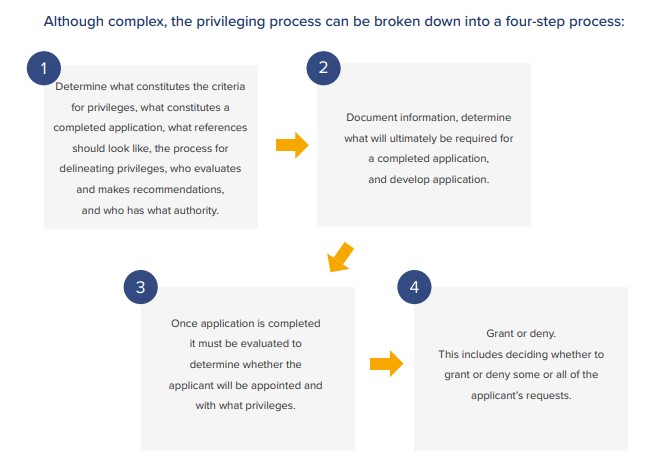
Process
With specific procedures in place, you’ll gain a structure for all the important steps in your privileging process, such as your exact decision-making methodology and how you communicate throughout it. When mapping out your process, you must consider every element of clinical privileging including the:
- Delineation
- Request
- Recommendation
- Granting
- Monitoring
- Eventual lookup of provider privileges
Go Manual or Automate?
The credentialing and privileging process is complex, time-consuming, and detail intensive. While implementing a manual process for your ASC is not out of the question, many organizations have found implementing a software solution saves time and increases quality. Pulling the content required for credentialing and privileging from disparate sources can be a tedious task. A software solution that comes with out of the box content – including privileging forms created specifically for your care setting and prebuilt credentialing and privileging workflows – will save you time and money. Software can also help prepare your organization for audits, securely store current/reliable provider information, and ensure that all documents and accreditations are easy to find and remain secure.
It’s important to realize that there is a lifecycle associated with the management of your providers’ competency and how you ensure clinical excellence at your surgery center. Software can help you answer questions like “how many” and “how well” and track other key performance metrics including clinical activity, general performance indicators, specialty-specific indicators, clinical case review results, and benchmarks. This type of data analysis is virtually impossible without some form of automation.
In Summary
As the government and payers scrutinize costs and push the shift to value-based care, outpatient surgery is expected to see an overall 11 percent increase from 2017 to 2022. If you’re operating an ASC – the time to get things right is NOW.
All ASCs are required by law to have some type of credentialing and privileging process in place. Some states are governed by state licensure, others require third party accreditation, and some must comply with both. All ASCs must meet CMS’ Conditions for Coverage (CfCs) to receive payment. But compliance is only one part of the equation. Setting up a first-rate credentialing and privileging process can position you as an ASC of choice. An online electronic process that is easy to complete results in provider satisfaction and enables you to readily recruit and retain top talent. Top talent will improve your reputation and result in increased business. Implementing an efficient privileging process doesn’t have to be hard – we’re here to help!
