June 8, 2022
June 8, 2022
High-quality cardiopulmonary resuscitation (CPR) can be a critical life or death determinant, but the last few years have made it clear that retaining, teaching and evaluating the skills required for CPR is perhaps more difficult than healthcare leaders and educators had previously understood. Specifically, accurately evaluating CPR skills can be an enormous challenge for educators.
Recent studies have concluded that the standard recommendation for 4 hours of training every two years for CPR and Automated External Defibrillator (AED) may not be sufficient. The studies cited a substantial deterioration of skills considerably before the two year mark.
Leveraging Technology to Ensure High Quality CPR
So, what is the best way to ensure that CPR skills are being properly taught and assessed across an organization? Do we have an accurate, measurable way to be sure that high-quality CPR can be consistently provided across the entire organization?
Healthcare leaders have multiple options for CPR training: 1) the traditional, instructor-led and instructor-observed classroom model, 2) instructorless models that use online content and manikins to evaluate and reinforce skills or, 3) a blended model that consists of online content with skills verified by an instructor.
First, it is important to understand some of the challenges of assessing the critical components of CPR. Some recent studies show that relying on instructor assessments of these skills can be problematic.
High quality CPR has four key components that educators need to accurately assess:
- Are students maintaining adequate chest compression fraction – providing compressions with minimal interruption?
- Are students achieving adequate depth (5 cm) and rate (100-120 per minute) of chest compressions?
- Are students allowing full recoil by avoiding leaning on the chest?
- Are students avoiding excessive ventilation (remaining between 8-10 breaths per minute)?
Studies suggest that manikins that can provide accurate feedback on all four key measures could be part of the solution in driving accuracy and consistency when a cardiac emergency occurs.
Evaluation Metrics
When taking a closer look at instructor-led performance and the efficacy of instructor evaluation, it is important to understand how instructors perform on some key metrics. First, the metrics themselves
- in order to best understand performance, it is important to look at instructor sensitivity and instructor specificity.
Instructor sensitivity is when the instructor accurately “passes” a learner on an assessment that should have passed as judged by objective manikin data. As an example, think of compression depth. If 60 learners perform compressions in the correct depth range as judged by a manikin, and the instructor passes 55 of the 60, instructor sensitivity would be 0.92. Instructor sensitivity is the proportion of the learners that were accurately passed by the instructor that should have passed based on an objective measure.
Instructor specificity is the accuracy in “failing” learners that should have failed on an assessment when compared to an objective criterion such as manikin data. For example, if 100 assessments were judged by manikin data to fail and the instructor failed 25 of them, instructor specificity is low—it would be 0.25.
Is it Possible to Accurately Assess Key CPR Performance Metrics?
A 2016 Danish study helped bring the challenges of accurate CPR skills assessment into sharper focus. (Hansen, 2019) The purpose of the study was to “investigate certified BLS instructors’ assessment skills in terms of identifying adequate and improper performances of chest compressions and rescue breathing.” (p. 281)
After completing a four-hour training course, all learners were assessed using a manikin. In addition, two instructors also assessed learners. The differences between the two assessments was striking. The manikin’s pass rates on the four critical components of CPR was dramatically lower for every measure.
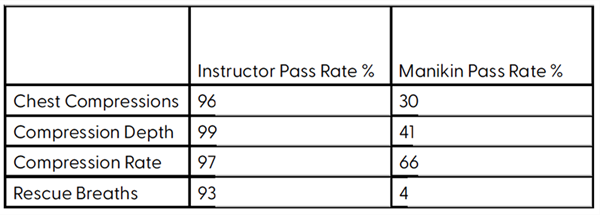
From these results, Danish researchers made these conclusions:
- Instructors were very good at passing learners that performed in correct ranges; however, they did a very poor job in identifying learners that performed outside of acceptable ranges.
- The use of instructor assessment may not be accurate enough to determine learner CPR skills in resuscitation research and that manikin data should be used whenever possible.
- Overall CPR quality was poor.
- BLS certificates may be awarded inappropriately by instructors possibly leading to inadequate performance in real-life conditions and affect survival negatively.
Somewhat similar research conducted by German researchers in 2019 reached a similar set of conclusions.
The German researchers compared results from two groups of learners. One hundred and twelve medical students were randomized to a control and an intervention group. All participants participated in a 30 minute lecture on the basics of CPR. Next, the control group participated in a 90 minute, instructor-led session of hands-on training. The intervention group took part in a 45 minute problem-based learning (PBL) session that was followed by 45 minutes of high fidelity simulation training. The PBL method helped instructors incorporate complex, real-life scenarios to help students more effectively learn CPR as well as helping to develop the critical thinking and communication skills that can be significant factors in a crisis.
Nearly 52% (51.9) of the intervention group met the established criteria for highquality CPR as opposed to just 12.5% of the control group. The German researchers concluded that simulation training led to a measurable increase in student’s ability to initiate high-quality CPR.
Researchers also noted that at the six month mark, the differences were considerably less pronounced.
They further concluded that the use of PBL with manikins led to measurable short-term increases in initiating sufficient CPR and went on to recommend periodic self-guided training using manikins to maintain adequate CPR skills.
We believe instructors continue to play a critical role in our healthcare
system and want to ensure their efforts are directed the highest use
of their time for providing the best patient care. By utilizing highly accurate feedback manikins to assess and document the critical performance metrics of CPR, you can ensure the best possible adherence to resuscitation guidelines, while also saving your organization money. on all four critical components of CPR results in more accurate evaluation of those skills.
Summary:
It is likely that CPR instruction that relies exclusively on instructor evaluation of performance will result in under-prepared providers. Technology, specifically manikins that can provide reliable feedback on all four critical components of CPR results in more accurate evaluation of those skills.
Benefits of The American Red Cross Resuscitation Suite™
- Adaptive learning tailored to individual needs
- On-demand learning accessible 24/7
- Incorporation of ILCOR and CoStar science recommendations
- Broader science including more than just resuscitation –
American Red Cross Scientific Advisory Council, Surviving Sepsis,
American College of Obstetricians and Gynecologists, etc. - Improved consistency through online learning
- Self- directed feedback mannikins
- Promotes consistent performance throughout organization
- Continual product improvement
- Focus on care provider safety
- Lower cost compared to other available products
- Student specific and efficient education leads to less classroom time and more bedside time
References
- Hansen, C., Bang, C. , Staerk, M. , Krogh, K. , & Lofgren, B. (2019). Certified basic life support instructors identify improper cardiopulmonary resuscitation skills poorly: Instructor assessments versus resuscitation manikin data. Simulation in Healthcare, 14, 281-286.
- Berger, C., Brinkrolf, C.E., Becker, J., Friederichs, H., Wenk, M., Van Aken, H., Hahnenkamp, K. (2019) Combination of problem based learning with high-fidelity simulation in CPR training improves short and long-term CPR skills: a randomised single blinded trial. BMC Medical Education
- Riegel, B., Nafziger, S. D., McBurnie, M., Powell, J., Ledingham, R., Sehra, R., Mango, L., Henry, M., PAD Trial Investigators. (March 2006) How well are cardiopulmonary resuscitation and automated External Defibrillator skills retained over time? Results from the Public Access Defibrillator (PAD) trial. Academic Emergency Medicine Journal, (March 2006) Vol. 13, No. 3, 254-263.

.png?sfvrsn=3028f62b_0)