

March 22, 2022
March 22, 2022
Turnover among nurses was a problem jeopardizing quality of patient care long before the pandemic hit in early 2020. Not only were hospitals in certain parts of the U.S. already experiencing severe nursing shortages, but they were also reeling from an unprecedented number of retirements among Baby Boomers who were leaving the workforce. The last thing the healthcare industry needed was something like a pandemic to make conditions worse for nurses and lead more than one in five to say they will leave bedside care entirely by the end of this year. Here are some startling statistics posted by The Advisory Board during their 2021 national meeting:
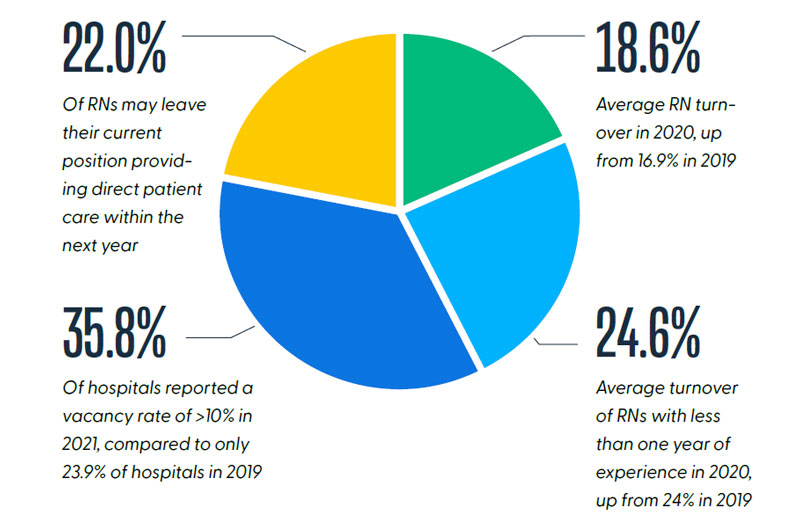
Source: “Hard Truths for CNOs: The Current & Future State of the Nursing Workforce,” Nursing Executive Center 2021 National Meeting, The Advisory Board.
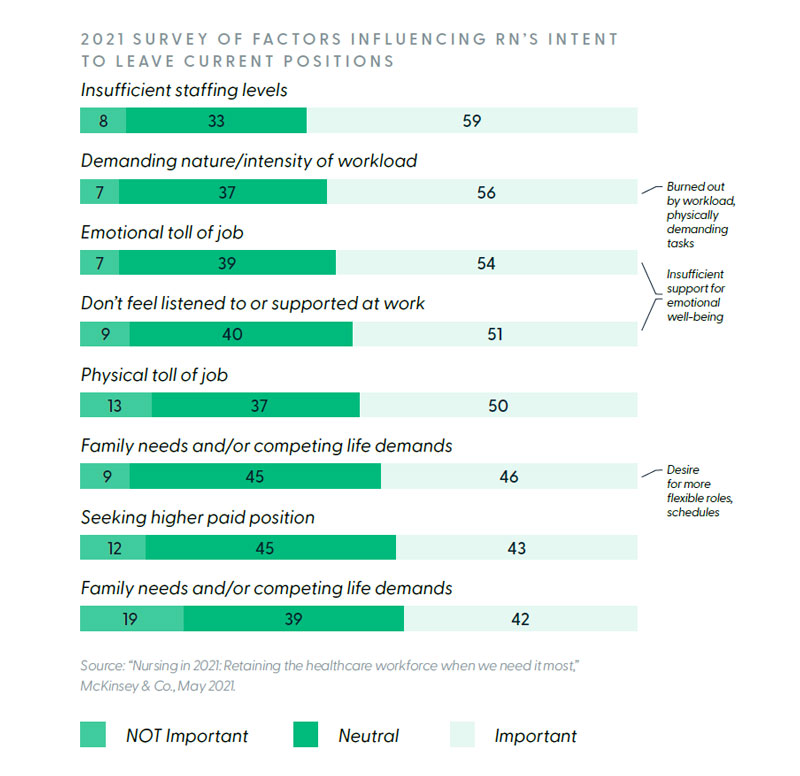
A recent study by McKinsey & Co. sheds some light on what is behind this flight from the bedside. According to their findings, two key factors are influencing nurses’ decisions to leave patient care. First, nurses feel burned out by workload and physically demanding tasks. Second, nurses feel insufficient support for their emotional well-being.
Unfortunately, it is hard to imagine a U.S. hospital today that is not faced with the dual challenges of addressing nurse burnout and well-being. All organizations are in the position of having to face these struggles and devise appropriate coping strategies. In the remainder of this article, HealthStream talks with two healthcare executives who are leading education and development efforts for their medical centers during this trying time. Specifically, HealthStream wanted to know the magnitude of the challenge at each organization, the priority being given to addressing nurse well-being, the strategies and tactics that were being implemented, and the impact their actions were having on overall quality of patient care. HealthStream spoke with Ambra Starr, RN, Nurse Education Coordinator, Peterson Regional Medical Center in Kerrville, TX and Craig Smith, Director of Education, Kingman Regional Medical Center, Kingman, AZ.
Both Starr and Smith confirm that their organizations, like those nationally, have seen spikes in nurse burnout since early 2020.
Smith reports that Kingman Regional has seen roughly 50% higher levels of burnout over the past two years as nurses fight to cope with “the marathon of it all.” He remarks that with this increase has come a subsequent rise in turnover.
Starr noted that the level of unease among nurses at the beginning was a result of fear of COVID-19 and was initially met by her team with education and coaching on resiliency. As the pandemic wore on though, burnout began to increase. Today, after going through the third and fourth waves of COVID-19 and caring for large numbers of patients who were lost, Starr states that “nurses were going beyond burnout into a more serious trauma response.”
Leaders in both hospitals quickly put nurse well-being as Priority One for their organizations. “I think well-being is everything. I really do,” says Smith. “If the primary needs of our staff aren’t met, secondary needs don’t matter.” Starr feels similarly, “Well-being has to be priority one, or you can’t care for others…our staff have to continue to do the work. They have to be able to go home and continue to be a husband, a father, a mom, a sister, a wife, a girlfriend, an aunt. Those things have to continue on. If staff are not whole, they cannot take care of those areas of their lives. Then, they can’t do the kind of work that they want to do first and foremost, and that our patients deserve.”
As the pandemic progressed, leadership in both organizations began to be more visible to staff and sought to provide support in ways that would build trust. It was a challenge to provide real support that would be meaningful to staff. According to Smith, “Cakes and treats and cookies are wonderful, but that’s not what our staff needs right now. What they want is help and support.” Both leadership teams wanted to be seen on the floors helping and supporting their caregivers.
Smith and his team of six educators believe trust between providers and educators is key. “We’ve gotten very creative with our education… we’ve been doing microlearning. We’ve certainly been relying on HealthStream for lectures and modules. We’ve been doing all kinds of creative things to try to support the nurses so they know they can trust us. My educators have been on the floors helping. They’re not sitting back here every day educating, they’re going up and doing support. They’re relieving nurses for lunches. They’re doing patient care sometimes. For over two years, we’ve gone up to ICU to help prone patients who are on ventilators. We’re out there with them fighting the fight, building that trust, building that relationship.”
Meaningful support programs have been put in place in both hospitals. At Peterson Regional, support began with a series of resiliency sessions, lasting about two hours each. “We wanted to start talking with our staff about burnout and resiliency. We wanted to give staff space to talk about the things they were scared of. What we know is when you don’t own what is keeping you up at night, then it continues to keep you up at night…We wanted to talk about how not to stay in that place and how to propel yourself out of that place so we can a) do the work that we know we’re going to have to do, and b) make sure that we’re taking care of ourselves.”
As burnout began morphing into a more serious trauma response, Peterson Regional brought in a trauma counselor. Starr reports, “She comes in two to four days a week, depending on what’s going on and what the needs are. She comes up sometimes at 10 o’clock at night and stays until two or three in the morning to work with our night staff. They all have her cell phone numbers. She’s got magnets around all of the departments, all of the patient units, because it’s not just that frontline staff that needs her help. Our staff can text her or meet with her in-person if they need to have a de-brief session.”
Kingman Regional also has implemented a full push to support staff. Pastoral care staff is doing regular rounding. Zoom sessions are available as needed with psychiatric experts, and meditation areas have been created within the hospital.
Training needs have also been adapted to fit the new environment. One surprise during the pandemic in both hospitals has been the experience of new nurses who have started their careers since the pandemic began. During their nurse residency programs, new staff began expressing concern about their ability to do “normal” nursing since all of their experience had been in the COVID-19 era. For example, one nurse mentioned that she doesn’t do IVs anymore. “I haven’t done IVs really pretty much ever because all of my COVID-19 patients have a PIC line. I don’t remember what to be worried about with a patient with congestive heart failure. I’m worried about what to do during regular codes, because all I know are intubation breathing codes.” Both Peterson and Kingman Regional now have refresher programs to bring these new employees up to speed.
Starr talks in general about the positive impact HealthStream’s Nurse Residency Program has had on new nurses. “It has been hugely impactful especially through this time to have that group of people all doing the same things. They are continuing to push each other, to grow each other, and to learn from each other…You have those reflection times at the beginning of the class, and they’re like, ‘I don’t know if I can do this. I don’t know if I can continue.’ Having that person saying, ‘You know what? I worked with you on that shift and you thought you were floundering, but that’s not what I saw. Here’s what I saw.’”
Both Starr and Smith speak to the positive impact their focus on well-being has had on their medical centers. Both point to the stability of their core measures and safety metrics and give credit to their supportive cultures and cohesive staff for their ability to weather the COVID-19 storm together. Starr comments, “We have worked really hard on the culture. Is it perfect? No. No culture is. Are there bad days? Yes, but when I took this job almost eight years ago, we really started focusing as an administrative team on the culture. When your culture is where it needs to be, your results are where they need to be. So stop looking, stop trying to work at results and start trying to focus on the people and the feel in the place and those things will happen. And it’s true and it has. It’s a lot of work and it’s hard, but it’s also worth it.”
Smith concludes, “I certainly think we’re headed in a positive direction. I try to be an optimist in everything I do. I really think that when COVID-19 slows down and we start to sit back finally and reflect, even though there’s going to be a lot of bad, I think a lot of good is going to come out of this too. This whole experience has really put the spotlight on training and development…And everything comes back to trust. Because if our staff trust me and I trust them, when things get bad, i.e., COVID, we’re going to work together.”
Read more about building back the workforce

.png?sfvrsn=3028f62b_0)